How Mounjaro Differs From Ozempic at a Molecular Level
If you’ve heard friends comparing Mounjaro and Ozempic, you’re not alone — both support weight loss and blood sugar control, but they work slightly differently under the skin. Understanding their molecular differences can help you make sense of how they feel in day-to-day use and why one might suit you better than the other.
At heart, both medicines are designed to enhance the actions of “incretin” hormones — natural signals that help your body manage appetite and blood sugar after meals. Ozempic contains semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1 RA), while Mounjaro contains tirzepatide, which activates both GLP-1 and a second incretin receptor called GIP (glucose-dependent insulinotropic polypeptide). That dual action is the key molecular difference — and it shapes how each medicine works in the body.
The Receptors: GLP-1 vs GLP-1+GIP
GLP-1 and GIP are hormones released from the gut after eating, prompting the pancreas to release insulin when glucose is high and generally helping stabilise blood sugar. Semaglutide (Ozempic) is a highly engineered mimic of GLP-1 that binds the GLP-1 receptor to trigger those pathways, including appetite signals in the brain and slower stomach emptying. Tirzepatide (Mounjaro) is different: it’s a “dual agonist” that binds both the GLP-1 receptor and the GIP receptor, combining the effects of both incretin systems in one molecule.
Researchers describe tirzepatide as “imbalanced” towards GIP — it has strong affinity and potency at the GIP receptor and somewhat weaker GLP-1 receptor potency compared with native GLP-1 or selective GLP-1 drugs. This deliberate design allows high engagement of GIP pathways while keeping GLP-1 engagement at tolerable levels, which may help with efficacy and comfort during dose increases.
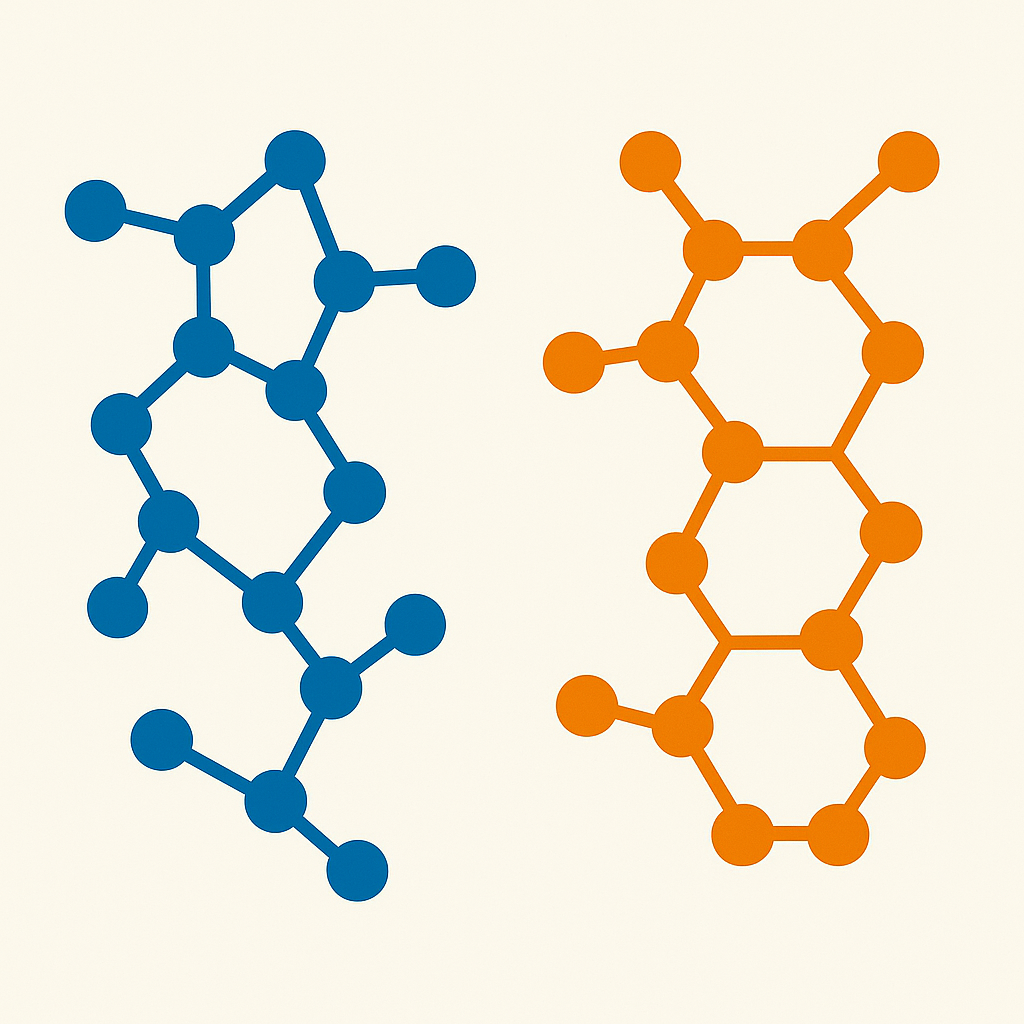
Molecular Design and Binding: What the Molecules Look Like
Semaglutide is closely based on human GLP-1 (about 94% similar), with small substitutions that make it resistant to breakdown and a fatty side-chain that helps it bind to albumin in the blood, giving a long half-life for once-weekly dosing. Tirzepatide is built on the GIP backbone (39 amino acids) with added features, including a C20 fatty di-acid chain, to engage both receptors and stay in the bloodstream long enough for weekly dosing.
These structural tweaks aren’t cosmetic — they shape how strongly and how long each drug binds its target. Semaglutide is a potent GLP-1 receptor activator, while tirzepatide shows near-native GIP receptor potency but lower GLP-1 receptor potency, yet still achieves clinically meaningful GLP-1 engagement at typical doses. In practical terms, tirzepatide’s blood levels at therapeutic doses are high enough to robustly activate GIP receptors and sufficiently activate GLP-1 receptors at the same time.
Signalling “Flavour”: How Messages Inside Cells Differ
When these drugs bind their receptors, they trigger signalling cascades inside cells — think of it as pressing buttons that release insulin or reduce appetite. Both semaglutide and tirzepatide raise cAMP inside pancreatic beta cells, boosting glucose-dependent insulin release and damping down glucagon, but their signalling “bias” can differ. Studies suggest tirzepatide shows biased signalling at the GLP-1 receptor, favouring cAMP over pathways tied to receptor internalisation, and behaves as a partial GLP-1 agonist while remaining a full GIP agonist. This nuanced signalling may contribute to its clinical profile alongside the dual-receptor effect.
A useful way scientists compare drugs is by “receptor occupancy” — how much of a receptor population is engaged at a given dose. Modelling indicates tirzepatide needs lower GLP-1 receptor occupancy than semaglutide to deliver similar glucose and weight effects, implying that engaging GIP adds to the overall benefit. This helps explain why a dual-agonist can outperform a pure GLP-1 drug at comparable tolerability levels in some studies.
Why Dual Agonism Might Matter for Weight and Glucose
By engaging GIP and GLP-1 together, tirzepatide can potentially amplify insulin release when glucose is high, further curb glucagon, and influence appetite and energy balance through complementary gut–brain signals. Semaglutide, as a selective GLP-1 RA, powerfully targets GLP-1 pathways, which are well known to lower appetite, slow gastric emptying, and improve beta-cell function. The dual-pathway approach of tirzepatide appears to provide additional leverage, likely explaining head-to-head findings where tirzepatide has shown superior efficacy over semaglutide in several outcomes, even though the GLP-1 component is less potent on its own.
Expert Insights
“Combining GLP-1 and GIP actions in a single molecule can enhance glucose control and weight effects while keeping GLP-1 exposure at tolerable levels,” notes findings from a detailed pharmacology analysis of tirzepatide’s receptor engagement and signalling profile. As another review puts it, semaglutide is a highly potent GLP-1 analogue with structural changes for once-weekly dosing and robust appetite-regulating effects via GLP-1 pathways.
Real-World Experiences
People often describe an appetite shift with both medicines, but the nuance can vary. One UK user shared that, after two weeks on a dual-agonist, their “food noise” eased more than with a prior GLP-1-only medicine — they felt satisfied sooner and thought about snacks less, which made meal planning easier. Others on semaglutide describe steady appetite reduction and smaller portions over time, aligning with its strong GLP-1 receptor activation and central effects.
Practical Implications: What You Might Notice
At a molecular level, semaglutide delivers a focused GLP-1 signal, while tirzepatide blends strong GIP signalling with moderate GLP-1 signalling. For you, that could translate to differences in how quickly appetite settles, how full you feel after meals, and how glucose responds to food — especially as doses rise. Not everyone experiences these changes the same way, and both medicines are designed for gradual dose escalation to help your body adjust.
- If you’ve done well on a GLP-1-only medicine but want more, dual agonism may offer an extra nudge by recruiting the GIP pathway.
- If you’re sensitive to GLP-1 effects like nausea, a medicine designed to favour GIP engagement while moderating GLP-1 occupancy may feel gentler as you titrate.
Risks & Considerations
Common effects like nausea or reduced appetite are linked to GLP-1 receptor activation, and careful dose increases help most people adjust; the GIP-favouring design of tirzepatide aims to balance efficacy with tolerability. Always follow the dosing schedule provided and speak with a clinician if side effects persist or feel concerning.
Key Takeaways
- Ozempic (semaglutide) is a selective GLP-1 receptor agonist; Mounjaro (tirzepatide) activates both GIP and GLP-1 receptors.
- Tirzepatide is intentionally “imbalanced” toward GIP, with strong GIP receptor potency and moderate GLP-1 receptor potency, yet therapeutic doses engage both.
- Semaglutide closely mimics GLP-1 with structural tweaks for once-weekly dosing and potent GLP-1 signalling in the brain and pancreas.
- Dual agonism can enhance glucose control and weight effects beyond GLP-1 alone by combining complementary incretin pathways.
- Individual responses vary; dose titration helps balance benefits and tolerability across both medicines.
You’ve taken a positive step by learning how these medicines differ — keep the conversation going with your healthcare professional to find the best fit for your goals.
For pricing and availability, check our price comparison tool.
Sources
- Tirzepatide — NCBI Bookshelf
- GLP-1 Receptor Agonists / Semaglutide: Clinical Overview — NCBI Bookshelf
- Tirzepatide’s dual GIP/GLP-1 receptor pharmacology — JCI Insight
- Mechanistic profile of tirzepatide: dual incretin agonism — Frontiers in Endocrinology (2024)
- Pharmacokinetic–pharmacodynamic modelling of dual incretin therapy — PubMed Central (Open Access)
- GIP and GLP-1 co-agonism for obesity and diabetes — Frontiers in Endocrinology (2022)
- Dual incretin agonists in metabolic disease — Signal Transduction and Targeted Therapy (Nature Portfolio)
- Incretin physiology and therapeutic targeting — PubMed Central (Review)
- Biased agonism at the GLP-1 receptor — Nature Communications
- Ozempic (semaglutide): Mechanism of Action — Novo Nordisk (Novomedlink)