The Dual Hormone Approach of Tirzepatide Explained
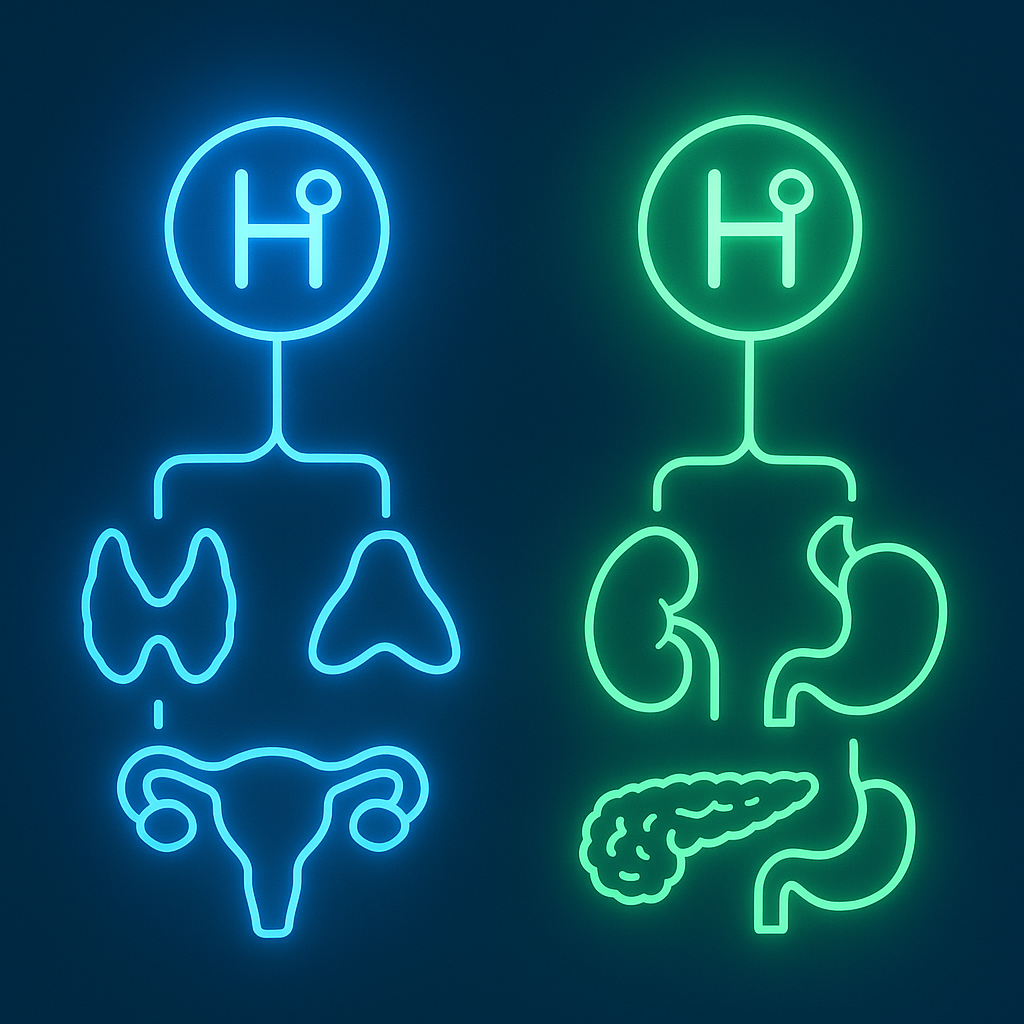
Tirzepatide has emerged as a groundbreaking medication that takes a dual hormone approach to managing both diabetes and weight. Rather than targeting just one hormone system like traditional treatments, tirzepatide harnesses the power of two key gut hormones simultaneously, creating what scientists call a “twincretin” effect. This approach represents a significant advancement in metabolic medicine, offering enhanced benefits for glucose control and weight management compared with single-hormone treatments.
The dual hormone mechanism works by mimicking both GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide), two naturally occurring incretin hormones released after meals. These hormones help the body manage blood sugar and appetite, but when combined in tirzepatide’s formulation, they create complementary effects that go beyond what either hormone achieves alone.
Understanding the Two Hormone Systems
GLP-1 and GIP belong to a family of hormones called incretins, which act as messengers between the digestive system and other organs. Both are released from specialised intestinal cells when you eat, but they work in distinct yet complementary ways to maintain metabolic balance.
GLP-1, secreted from L-cells in the lower intestine, stimulates insulin release, suppresses glucagon (a hormone that raises blood sugar), slows gastric emptying, and reduces appetite. These effects make GLP-1 receptor agonists well-established options for diabetes management and weight loss.
GIP, produced by K-cells in the upper intestine, was once called “gastric inhibitory peptide” but is now understood as “glucose-dependent insulinotropic polypeptide”. It also stimulates insulin secretion, modulates glucagon in a glucose-dependent manner, and influences fat metabolism. GIP’s effects can vary with blood glucose levels and broader metabolic context.
Key differences between GLP-1 and GIP include:
- GLP-1 consistently suppresses appetite and promotes weight loss, whilst GIP’s appetite effects are more context-dependent.
- GLP-1 generally inhibits glucagon, whilst GIP can stimulate or inhibit glucagon depending on glucose levels.
- GLP-1 slows gastric emptying more prominently than GIP.
- GIP has additional effects on fat cells and bone metabolism not seen with GLP-1.
- GIP receptors are widely distributed, including on adipose tissue.
- GLP-1’s insulinotropic effects are preserved in many people with type 2 diabetes, whereas GIP responsiveness may be reduced.
The Synergistic Advantage
Tirzepatide’s dual hormone approach creates synergistic effects that exceed the sum of its individual components. In clinical studies, tirzepatide has produced superior weight loss and glucose control compared with selective GLP-1 receptor agonists at their maximum doses.
The mechanism behind this enhanced effectiveness lies in how the two hormone systems complement each other. GLP-1 provides robust appetite suppression and glucose control, while GIP may amplify these benefits through different pathways. Early research also suggests GIP activation could reduce some gastrointestinal adverse effects associated with GLP-1 stimulation, potentially improving treatment tolerance.
Clinical advantages of the dual approach include:
- Greater weight loss (typically in the 20–22% range versus ~13–15% with GLP-1 agonists alone, depending on study and population).
- Enhanced glucose control, with more patients achieving normal HbA1c levels.
- Improved insulin sensitivity beyond GLP-1 alone.
- Favourable effects on cardiovascular risk factors such as blood pressure and lipids.
- Potentially better long-term sustainability due to tolerability advantages.
- In some patients, a reduced risk of treatment-related side effects.
Studies indicate that tirzepatide works through both direct and indirect pathways. It directly activates receptors on pancreatic β-cells to enhance insulin secretion and indirectly modulates α-cells to fine-tune glucagon release. Together, this provides more comprehensive metabolic control than single-hormone treatments.
Expert Insights
“The improved performance is likely linked to tirzepatide’s dual mechanism of action. Whereas semaglutide works by activating GLP-1 receptors, tirzepatide mimics not only GLP-1 but also GIP. Together, these actions reduce hunger, lower blood-glucose levels, and affect fat-cell metabolism.”
Health technology assessments have also noted statistically significant reductions in HbA1c and weight across multiple trials. Experts highlight relatively flat HbA1c dose–response curves, meaning effective glucose control can often be achieved at lower doses—another potential tolerability advantage of the dual approach.
User Experiences
Real-world experiences often mirror clinical findings. People commonly report strong appetite control, fewer cravings, and steady early weight loss, while many also describe pens as straightforward to use and side effects as manageable.
Practical strategies for maximising dual-hormone benefits:
- Start low and increase gradually so your body can adjust to both hormone systems.
- Keep regular meal times to support natural incretin rhythms.
- Focus on balanced nutrition rather than strict restriction; the medicine helps regulate portions.
- Track glucose and weight to monitor comprehensive metabolic changes.
- Stay consistent with weekly dosing to maintain steady hormone levels.
- Work with your clinician to adjust the dose based on response and tolerability.
Understanding the UK Medical Context
In the UK, tirzepatide is recognised as a novel dual GIP/GLP-1 receptor agonist for type 2 diabetes and weight management. NICE guidance and NHS England implementation materials describe clinically meaningful reductions in HbA1c and weight across trials and outline how access should be rolled out within services. The dual-hormone mechanism is highlighted as a new therapeutic approach that requires careful, equitable implementation.
Key Takeaways
- Tirzepatide uniquely combines GLP-1 and GIP actions, delivering synergistic effects for glucose control and weight management.
- Clinical outcomes are often superior, with many patients achieving substantial weight loss and tighter glycaemic control than with GLP-1 alone.
- Complementary pathways regulate appetite, glucose, and metabolism, which may also support tolerability.
- UK guidance sets out who may benefit and how services should implement access safely and fairly.
Understanding tirzepatide’s dual-hormone approach helps explain why it is viewed as a major advance in metabolic health, offering a more comprehensive option for people managing diabetes and obesity.
For pricing and availability, check our price comparison tool.
Sources
- Tirzepatide for managing overweight and obesity — NICE Technology Appraisal TA1026
- Interim commissioning guidance for tirzepatide implementation — NHS England (March 2025)
- MHRA authorises tirzepatide for weight management — UK Government
- GLP-1 medicines for weight loss and diabetes: what you need to know — UK Government
- Comparative weight-loss and glycaemic outcomes with tirzepatide vs GLP-1 agonists — JAMA Network Open
- Tirzepatide clinical trial results (SURPASS programme) — The Lancet
- Mechanistic insights into dual GIP/GLP-1 agonism — Nature Metabolism
- Incretin receptor signalling and metabolic effects — Science Advances
- Incretin system and physiology overview — NCBI Bookshelf
- GLP-1 physiology and therapeutic actions — PubMed